Overview

Pes planus can be part of normal development. Infants typically have a minimal arch. Many toddlers have flattening of the long arch, with forefoot pronation and heel valgus on weight-bearing. There may be ligamentous laxity, which is probably determined genetically. Most of these children spontaneously develop a strong normal arch by around age 10.
Causes
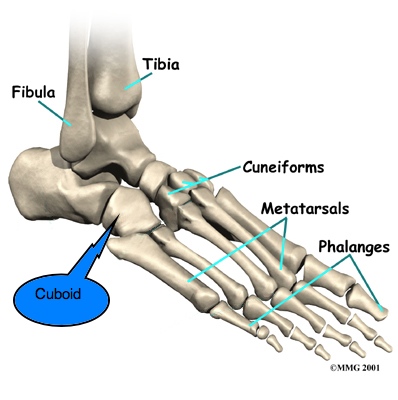
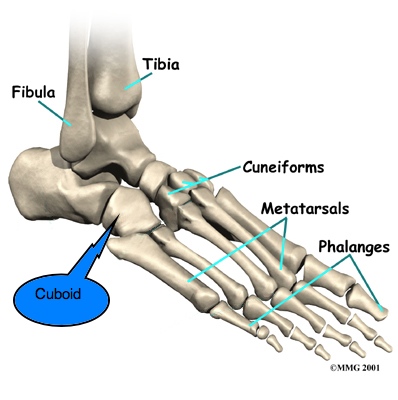
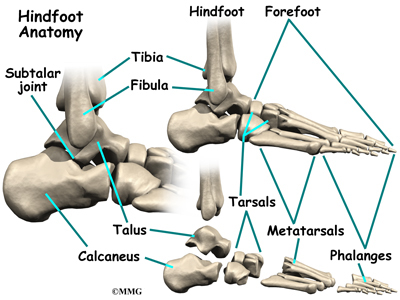
Flat feet in adults can arise from a variety of causes. Here are the most common. An abnormality that is present from birth, stretched or torn tendons, damage or inflammation of the posterior tibial tendon (PTT), which connects from your lower leg, along your ankle, to the middle of the arch, broken or dislocated bones. Some health conditions, such as rheumatoid arthritis, Nerve problems. Other factors that can increase your risk include obesity, diabetes, ageing and Pregnancy.
Symptoms
The primary symptom of fallen arches is painful or achy feet in the area in which the foot arches or on the heel. This area may become swollen and painful to stand still on. This causes the patient to improperly balance on their feet which in turn will cause other biomechanical injuries such as back, leg and knee pain.
Diagnosis
Your doctor examines your feet to determine two things, whether you have flat feet and the cause or causes. An exam may include the following steps, Checking your health history for evidence of illnesses or injuries that could be linked to flat feet or fallen arches, Looking at the soles of your shoes for unusual wear patterns, Observing the feet and legs as you stand and do simple movements, such as raising up on your toes, Testing the strength of muscles and tendons, including other tendons in the feet and legs, such as the Achilles tendon or the posterior tibial tendon, Taking X-rays or an MRI of your feet.
Non Surgical Treatment
Some patients with flat feet may automatically align their limbs in such a way that unpleasant symptoms never develop. In such cases treatment is not usually required. Pain in the foot that is caused by flat feet may be alleviated if the patient wears supportive well-fitted shoes. Some patients say that symptoms improve with extra-wide fitting shoes. Fitted insoles or orthotics (custom-designed arch supports) may relieve pressure from the arch and reduce pain if the patient's feet roll or over-pronate. The benefits of an orthotic only exist while it is being worn. Patients with tendonitis of the posterior tibial tendon may benefit if a wedge is inserted along the inside edge of the orthotic - this takes some of the load off the tendon tissue. Wearing an ankle brace may help patients with posterior tibial tendinitis, until the inflammation comes down. Rest, doctors may advise some patients to rest and avoid activities which may make the foot (feet) feel worse, until the foot (feet) feels better. A combination of an insole and some kind of painkiller may help patients with a ruptured tendon, as well as those with arthritis. Patients with a ruptured tendon or arthritis who find insoles with painkillers ineffective may require surgical intervention. Patients, usually children, whose bones did not or are not developing properly, resulting in flat feet from birth, may require surgical intervention to separate fused bones (rare). Bodyweight management, if the patient is obese the doctor may advise him/her to lose weight. A significant number of obese patients with flat feet who successfully lose weight experience considerable improvement of symptoms.
Surgical Treatment
This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer). Flat feet and fallen arches are common conditions that are in most cases asymptomatic. However, in patients who do have symptoms, treatments are available that can help reduce pain and promote efficient movement. Orthotic devices are well recognised as an excellent treatment and podiatrists can offer these different treatment modalities as individualised treatments for patients.
Prevention
Going barefoot, particularly over terrain such as a beach where muscles are given a good workout, is good for all but the most extremely flatfooted, or those with certain related conditions such as plantar fasciitis. Ligament laxity is also among the factors known to be associated with flat feet. One medical study in India with a large sample size of children who had grown up wearing shoes and others going barefoot found that the longitudinal arches of the bare footers were generally strongest and highest as a group, and that flat feet were less common in children who had grown up wearing sandals or slippers than among those who had worn closed-toe shoes. Focusing on the influence of footwear on the prevalence of pes planus, the cross-sectional study performed on children noted that wearing shoes throughout early childhood can be detrimental to the development of a normal or a high medial longitudinal arch. The vulnerability for flat foot among shoe-wearing children increases if the child has an associated ligament laxity condition. The results of the study suggest that children be encouraged to play barefooted on various surfaces of terrain and that slippers and sandals are less harmful compared to closed-toe shoes. It appeared that closed-toe shoes greatly inhibited the development of the arch of the foot more so than slippers or sandals. This conclusion may be a result of the notion that intrinsic muscle activity of the arch is required to prevent slippers and sandals from falling off the child?s foot.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.

Pes planus can be part of normal development. Infants typically have a minimal arch. Many toddlers have flattening of the long arch, with forefoot pronation and heel valgus on weight-bearing. There may be ligamentous laxity, which is probably determined genetically. Most of these children spontaneously develop a strong normal arch by around age 10.
Causes
Flat feet in adults can arise from a variety of causes. Here are the most common. An abnormality that is present from birth, stretched or torn tendons, damage or inflammation of the posterior tibial tendon (PTT), which connects from your lower leg, along your ankle, to the middle of the arch, broken or dislocated bones. Some health conditions, such as rheumatoid arthritis, Nerve problems. Other factors that can increase your risk include obesity, diabetes, ageing and Pregnancy.
Symptoms
The primary symptom of fallen arches is painful or achy feet in the area in which the foot arches or on the heel. This area may become swollen and painful to stand still on. This causes the patient to improperly balance on their feet which in turn will cause other biomechanical injuries such as back, leg and knee pain.
Diagnosis
Your doctor examines your feet to determine two things, whether you have flat feet and the cause or causes. An exam may include the following steps, Checking your health history for evidence of illnesses or injuries that could be linked to flat feet or fallen arches, Looking at the soles of your shoes for unusual wear patterns, Observing the feet and legs as you stand and do simple movements, such as raising up on your toes, Testing the strength of muscles and tendons, including other tendons in the feet and legs, such as the Achilles tendon or the posterior tibial tendon, Taking X-rays or an MRI of your feet.
Non Surgical Treatment
Some patients with flat feet may automatically align their limbs in such a way that unpleasant symptoms never develop. In such cases treatment is not usually required. Pain in the foot that is caused by flat feet may be alleviated if the patient wears supportive well-fitted shoes. Some patients say that symptoms improve with extra-wide fitting shoes. Fitted insoles or orthotics (custom-designed arch supports) may relieve pressure from the arch and reduce pain if the patient's feet roll or over-pronate. The benefits of an orthotic only exist while it is being worn. Patients with tendonitis of the posterior tibial tendon may benefit if a wedge is inserted along the inside edge of the orthotic - this takes some of the load off the tendon tissue. Wearing an ankle brace may help patients with posterior tibial tendinitis, until the inflammation comes down. Rest, doctors may advise some patients to rest and avoid activities which may make the foot (feet) feel worse, until the foot (feet) feels better. A combination of an insole and some kind of painkiller may help patients with a ruptured tendon, as well as those with arthritis. Patients with a ruptured tendon or arthritis who find insoles with painkillers ineffective may require surgical intervention. Patients, usually children, whose bones did not or are not developing properly, resulting in flat feet from birth, may require surgical intervention to separate fused bones (rare). Bodyweight management, if the patient is obese the doctor may advise him/her to lose weight. A significant number of obese patients with flat feet who successfully lose weight experience considerable improvement of symptoms.
Surgical Treatment
This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer). Flat feet and fallen arches are common conditions that are in most cases asymptomatic. However, in patients who do have symptoms, treatments are available that can help reduce pain and promote efficient movement. Orthotic devices are well recognised as an excellent treatment and podiatrists can offer these different treatment modalities as individualised treatments for patients.
Prevention
Going barefoot, particularly over terrain such as a beach where muscles are given a good workout, is good for all but the most extremely flatfooted, or those with certain related conditions such as plantar fasciitis. Ligament laxity is also among the factors known to be associated with flat feet. One medical study in India with a large sample size of children who had grown up wearing shoes and others going barefoot found that the longitudinal arches of the bare footers were generally strongest and highest as a group, and that flat feet were less common in children who had grown up wearing sandals or slippers than among those who had worn closed-toe shoes. Focusing on the influence of footwear on the prevalence of pes planus, the cross-sectional study performed on children noted that wearing shoes throughout early childhood can be detrimental to the development of a normal or a high medial longitudinal arch. The vulnerability for flat foot among shoe-wearing children increases if the child has an associated ligament laxity condition. The results of the study suggest that children be encouraged to play barefooted on various surfaces of terrain and that slippers and sandals are less harmful compared to closed-toe shoes. It appeared that closed-toe shoes greatly inhibited the development of the arch of the foot more so than slippers or sandals. This conclusion may be a result of the notion that intrinsic muscle activity of the arch is required to prevent slippers and sandals from falling off the child?s foot.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
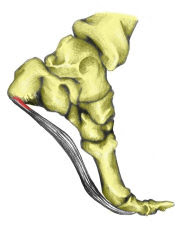






 The Achilles tendon is the largest tendon in the human body. It connects the calf muscle to the heel bone. However, this tendon is also the most common site of rupture or tendonitis, an inflammation of the tendon due to overuse. Achilles tendon rupture is a partial or complete tear of the Achilles tendon. It comes on suddenly, sometimes with a popping sound, and can be debilitating. A full rupture is more severe, but less common, than a partial rupture. A full rupture splits the Achilles tendon so that it no longer connects the calf muscle to the heel: the calf muscle can no longer cause the foot to push off, so normal walking is impossible. If it is a full rupture, then lightly pinching the Achilles tendon with the forefinger and thumb will reveal a gap in the Achilles tendon. Partial and full Achilles tendon ruptures are most likely to occur in sports requiring sudden stretching, such as sprinting and racquet sports. Partial Achilles tendon tears are also common among middle and long distance runners.
The Achilles tendon is the largest tendon in the human body. It connects the calf muscle to the heel bone. However, this tendon is also the most common site of rupture or tendonitis, an inflammation of the tendon due to overuse. Achilles tendon rupture is a partial or complete tear of the Achilles tendon. It comes on suddenly, sometimes with a popping sound, and can be debilitating. A full rupture is more severe, but less common, than a partial rupture. A full rupture splits the Achilles tendon so that it no longer connects the calf muscle to the heel: the calf muscle can no longer cause the foot to push off, so normal walking is impossible. If it is a full rupture, then lightly pinching the Achilles tendon with the forefinger and thumb will reveal a gap in the Achilles tendon. Partial and full Achilles tendon ruptures are most likely to occur in sports requiring sudden stretching, such as sprinting and racquet sports. Partial Achilles tendon tears are also common among middle and long distance runners.
 RSS Feed
RSS Feed